Psoriasis and eczema are two common skin illnesses that can be painful and have an impact on a person's quality of life. While their symptoms may be similar, they are distinct illnesses with distinct characteristics. This blog will look at the differences between Psoriasis and Eczema.
Identifying Psoriasis and Eczema
Recognising the unique signs and characteristics of psoriasis and eczema is required. While both illnesses can produce redness, itching, and discomfort, there are significant distinctions in their looks and patterns that can help distinguish them:
Psoriasis:
-
Appearance: Psoriasis is frequently characterised by thick, silvery scales over red patches of skin. The affected areas usually have well-defined borders between the lesions and the surrounding skin. Psoriasis is most commonly found on the scalp, elbows, knees, lower back, and nails. Plaque Psoriasis is the most common type, characterised by raised plaques on the skin.
-
Texture: Psoriasis-affected skin may feel thicker or more elevated due to the accumulation of skin cells.
-
Itching and Pain: Itching and pain are common symptoms of psoriasis, but the severity varies from person to person.
Eczema (Atopic Dermatitis):
-
Appearance: Eczema is typically characterised by red, inflamed patches that can be dry, scaly, or weepy. Eczema on the face, behind the knees, inside the elbows, and on the neck is common in infants and young children. Eczema patches can change their appearance over time, becoming crusty, blistered, or cracked.
-
Texture: Eczema-affected skin can feel rough, dry, and may have a rough texture due to scratching.
-
Itching: Eczema is characterised by severe itching. The desire to scratch might be overwhelming, causing more irritation and infection.
It is important to visit a healthcare practitioner or a dermatologist for an accurate diagnosis and proper therapy. Based on a visual examination, they can distinguish between psoriasis and eczema and, if necessary, may do additional tests or biopsies to confirm the diagnosis. Remember that both illnesses are chronic and must be managed properly. Treatment regimens will be personalised to the exact ailment, symptoms, and severity of each individual.
Key Symptoms of Psoriasis
Psoriasis is a chronic autoimmune condition that primarily affects the skin, causing rapid cell growth. The following are common psoriasis symptoms, which vary in severity and presentation depending on the individual:
-
Red Skin Patches: One of the main signs of psoriasis is the presence of raised, inflammatory, and red skin patches. These patches are frequently covered in silvery-white scales.
-
Silvery Scales: Thick, silvery-white scales cover the red patches in most cases. These scales form as a result of the rapid turnover of skin cells, which accumulate on the surface before the older cells shed.
-
Itching and Dryness: The affected areas may become dry, causing itching or irritation. Itching is common in psoriasis, which can lead to scratching and skin damage.
-
Thickened or pitted nails: Psoriasis can cause changes in the appearance of the nails. Nails may become thickened, ridged, discoloured, or pitted. In severe cases, nails may crumble or detach from the nail bed.
-
Joint Pain and Swelling (Psoriatic Arthritis): Psoriatic arthritis affects approximately 30% of people with psoriasis. This disease causes joint pain, stiffness, and swelling. It can affect any joint and can range in severity from mild to severe.
-
Burning or Soreness: Some people with psoriasis may experience burning or soreness in the affected areas.
-
Locations of Lesion: Elbows, knees, scalp, lower back, and nails are among the body parts where psoriasis frequently manifests. But it can happen anywhere on the body, including the face, soles of the feet, and palms.
-
Inverse Psoriasis: Due to the moist environment, this type of psoriasis affects skin folds such as the armpits, groyne, under the breasts, and genital areas, appearing as smooth, red patches without scales.
The degree of psoriasis symptoms can range from minor, with little patches of discomfort, to severe, with greater parts of the body affected. The illness is persistent, with periods of flare-ups and remission. A dermatologist or other healthcare expert should be consulted for an accurate diagnosis and to identify the best treatment plan to control and alleviate the symptoms of psoriasis.
Eczema: Signs and Symptoms
Eczema, also known as atopic dermatitis, is a chronic, inflammatory skin illness that most often affects children but can affect people of any age. Dry and itchy skin, red or inflamed skin patches, scaly or cracked skin, weeping or seeping lesions, sensitive skin, affected body parts, itch-scratch cycle, sleep difficulties, and lichenification are all signs and symptoms of eczema. Eczema symptoms can range in severity and may appear intermittently or consistently. Stress, allergens, particular foods, environmental conditions, or irritants can all aggravate eczema symptoms. If you suspect you or someone you know has eczema, consult a dermatologist or other healthcare expert right away. They can provide an accurate diagnosis and an individualised treatment plan for patients suffering from eczema to manage symptoms and enhance quality of life.
Diagnostic Criteria for Psoriasis and Eczema
Psoriasis and eczema (atopic dermatitis) are usually diagnosed clinically by a healthcare professional or dermatologist. While no specific laboratory tests are available to definitively diagnose these disorders, doctors rely on a mix of symptoms, medical history, and, in some cases, further testing to confirm the diagnosis. The general diagnostic criteria for psoriasis and eczema are as follows:
Psoriasis:
-
Clinical Examination: Healthcare professionals examine the skin, nails, and scalp for characteristic signs of psoriasis, including red patches with silvery scales.
-
Medical History: Doctors examine the patient's medical history to see if there is a family history of psoriasis or other related conditions, as well as the duration, location, and severity of skin lesions.
-
Physical Exam: They look for specific features such as the Auspitz sign (pinpoint bleeding when scales are removed), the Koebner phenomenon (new lesions forming at sites of skin injury), and various types of psoriasis lesions.
-
Biopsy (if necessary): When the diagnosis is unclear, a skin biopsy may be performed. To confirm the presence of psoriasis, a small sample of skin is removed and examined under a microscope.
Eczema (Atopic Dermatitis):
-
Clinical examination: Healthcare providers examine the skin for eczema symptoms such as red, itchy, and inflamed patches, as well as the distribution and appearance of lesions.
-
Medical History: Doctors inquire about any personal or family history of eczema or other atopic conditions such as asthma or allergic rhinitis, as these conditions frequently coexist.
-
Physical examination: They assess the condition of the skin, looking for specific features such as the presence of dry, scaly patches, weeping or crusted lesions, and affected areas on the body.
-
Exclusion of Other Conditions: Using clinical examination and tests, doctors can sometimes rule out other skin conditions that may mimic eczema.
-
Patch Testing (if required): Patch testing may be performed to identify specific allergens or irritants in cases where contact dermatitis is suspected as the cause of eczema-like symptoms.
It is important to note that psoriasis and eczema can have similar symptoms and may coexist, making an accurate diagnosis critical for effective treatment. If you suspect you have either condition, it's advisable to seek medical advice from a dermatologist or healthcare professional for proper evaluation and management.
Treatment and Management Strategies
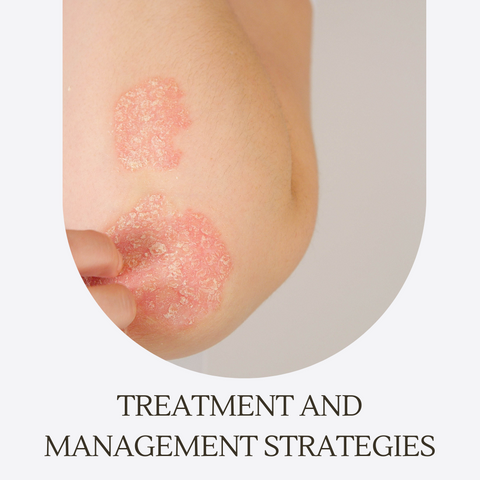
Psoriasis and eczema (atopic dermatitis) therapy and management options attempt to alleviate symptoms, reduce inflammation, prevent flare-ups, and enhance overall quality of life. Treatment strategies are frequently adapted to the severity of the ailment and the demands of the individual patient. Here are some common methods for treating psoriasis and eczema:
Psoriasis Treatment:
-
Topical Treatments: These anti-inflammatory creams or ointments aid in the reduction of itching and inflammation. These medications, derived from vitamin A, aid in slowing skin cell growth. These topical immunosuppressants are used on sensitive areas of the skin, such as the face or skin folds.
-
Phototherapy (Light Therapy): Skin cell growth can be slowed and inflammation can be reduced with medical supervision during controlled ultraviolet (UV) light exposure.
-
Oral Medications: To suppress the immune system or regulate skin cell growth in severe cases, oral medications such as methotrexate, cyclosporine, or retinoids may be prescribed.
-
Biologic Therapies: These newer medications, administered via injection or infusion, target specific immune system pathways involved in psoriasis.
-
Lifestyle Modifications: To relieve dry skin, moisturise regularly. Avoiding stress, certain medications, and skin injuries as triggers. Stress management can be accomplished through relaxation techniques or therapy.
Eczema Treatment:
-
Emollients and Moisturizers: Regular application of thick creams or ointments keeps the skin hydrated and reduces dryness and itching.
-
Topical Corticosteroids and Calcineurin Inhibitors: These medications help to reduce inflammation and itching in eczema-prone areas.
-
Antihistamines: These medications can help alleviate itching and improve sleep quality, particularly during flare-ups.
-
Avoiding Triggers: Identifying and avoiding eczema triggers such as specific soaps, detergents, allergens, or environmental factors.
-
Wet Wrap Therapy: Wrapping affected areas in damp bandages or clothing after applying moisturiser can help soothe and hydrate the skin during severe flare-ups.
-
Biologic Medications (for severe cases): Newer medications, such as dupilumab, are approved for moderate to severe eczema that has not responded to other treatments.
-
Behavioral Therapies: Cognitive-behavioral therapies or stress management techniques can help reduce stress, which can aggravate eczema symptoms.
In both cases, the treatment strategy may necessitate a combination of therapies tailored to the patient's specific needs. To find the best course of action and track the condition's development over time, speak with a dermatologist or other healthcare provider. Regular follow-ups and adjustments to the treatment plan may be required for optimal management.
Effective Treatments for Psoriasis
Psoriasis is a chronic autoimmune skin illness that cannot be cured. Several therapies are being developed to assist those suffering from the condition in managing their symptoms, reducing inflammation, and improving their quality of life. Because treatment success varies from person to person, a dermatologist or healthcare practitioner will usually adapt the treatment plan based on the kind, intensity, and location of the psoriasis. The following are some effective psoriasis treatments:
-
Corticosteroids, topical retinoids, calcineurin inhibitors, and coal tar preparations are examples of topical treatments.
-
UVB phototherapy and PUVA (Psoralen plus Ultraviolet A) phototherapy are two types of phototherapy (light therapy).
-
Oral retinoids, methotrexate, cyclosporine, and biological therapies are examples of systemic medications.
-
Other treatments include acitretin, apremilast, and a lifestyle change.
Effective psoriasis treatment frequently entails a combination of therapies tailored to an individual's specific condition and needs. Regular check-ins with healthcare professionals are essential for monitoring treatment efficacy, adjusting therapies as needed, and managing potential side effects.
Managing Eczema: Best Practices
To alleviate symptoms and enhance skin health, eczema, also known as atopic dermatitis, requires a combination of preventive measures, skincare regimens, and treatment tactics. Skincare and hygiene, avoiding triggers, treatment options, lifestyle adjustments, and regular check-ups are some of the best practices for treating eczema. Eczema management frequently necessitates a tailored strategy. What works for one person may not work for another, so working together with healthcare specialists to build an effective management plan tailored to individual needs is crucial.
Lifestyle Changes for Skin Health
Maintaining healthy skin entails adopting lifestyle habits that promote its well-being. Here are some lifestyle changes that can help improve skin health:
Diet and Hydration:
-
Stay Hydrated: Drink plenty of water every day to keep your skin hydrated from within.
-
Balanced Diet: To support skin health, eat a diet rich in fruits, vegetables, whole grains, and healthy fats (omega-3 fatty acids found in fish, flaxseeds, and so on).
-
Limit Sugar and Processed Foods: Excess sugar and processed foods can both contribute to inflammation and skin problems. The key word here is moderation.
Skincare Routine:
-
Gentle Cleansing: To avoid stripping natural oils, use mild, fragrance-free cleansers appropriate for your skin type.
-
Moisturise: Apply moisturisers or emollients regularly to keep the skin hydrated, especially after bathing or washing.
-
Sun Protection: Apply sunscreen with an SPF of at least 30 every day to protect your skin from UV rays, which can cause premature ageing and skin damage.
-
Avoid smoking: Smoking can cause skin collagen damage, resulting in premature ageing and wrinkles.
Stress Management:
-
Stress Management: Engage in stress-relieving activities such as meditation, yoga, or deep breathing exercises. High levels of stress can aggravate skin conditions.
-
Adequate Sleep: Get enough rest to allow your body and skin to repair and rejuvenate.
Healthy Habits:
-
Exercise regularly: Physical activity improves blood circulation, which benefits skin health by delivering nutrients and oxygen to skin cells.
-
Avoid Harsh Chemicals: Look for skincare products with gentle ingredients and steer clear of harsh chemicals that can irritate the skin.
-
Proper Hygiene: Bathe regularly, but avoid hot water and harsh soaps that can dry out the skin.
-
Avoid Picking or Scratching: To avoid further damage or infection, avoid picking at acne or scratching at skin irritations.
Regular Check-ups:
-
Consult a Dermatologist: Regular visits to a dermatologist can aid in the detection and treatment of skin problems.
-
Self-Examinations: Conduct regular self-examinations to detect any changes in moles, spots, or other skin abnormalities.
Environmental Considerations:
-
Protective Clothes: Dress appropriately to protect your skin from the elements, particularly from intense cold or sunlight.
-
Humidifiers: To maintain ideal humidity levels and avoid skin dryness in dry environments, use a humidifier.
Allergen Management:
-
Determine Triggers: Recognise and stay away from known allergens and irritants that can make skin disorders like contact dermatitis or eczema worse.
-
Allergy Testing: If allergies have a major negative influence on skin health, think about having an allergy test to determine particular triggers.
Making these lifestyle adjustments can have a big impact on having healthier skin. Individual skin types and conditions vary, so it is important to find a routine and habits that work best for your skin and seek professional advice if necessary.
Understanding the Impact on Daily Life

Psoriasis and eczema, as chronic skin illnesses, can have a major impact on an individual's daily life in a variety of ways due to their persistent symptoms, potential discomfort, and emotional toll. Here's an overview of how various illnesses can impact daily life:
Psoriasis Impact:
-
Physical Discomfort: Psoriasis symptoms such as itching, pain, and the presence of visible skin lesions can cause physical discomfort and impair mobility, especially if joints are involved (psoriatic arthritis).
-
Emotional Well-Being: Living with visible skin changes may cause feelings of self-consciousness, embarrassment, or low self-esteem, affecting social interactions and confidence.
-
Sleep Disturbances: Psoriasis itching and discomfort can disrupt sleep patterns, resulting in fatigue and a lower quality of life.
-
Daily Activities: Psoriasis lesions, particularly those on the hands, feet, or joints, can make it difficult to walk, use one's hands, or engage in certain exercises.
-
Social Impact: Social disengagement or situational avoidance may result from fear of criticism or stigma brought on by obvious skin changes.
Eczema Impact:
-
Excessive Itching: Itching associated with eczema can be extremely uncomfortable and long-lasting, making it difficult to focus on daily tasks.
-
Skin Discomfort: Dry, cracked, and inflammatory skin can make moving painful or uncomfortable by causing soreness, pain, or a burning feeling.
-
Sleep Disturbances: Itching and irritation can cause sleep disturbances, which can result in daytime weariness and a reduction in productivity.
-
Emotional Impact: The outward manifestations of eczema may cause stress, anxiety, depression, or feelings of self-consciousness that can negatively impact mental health.
-
Effect on Activities: Activities involving contact with irritants or triggers may be restricted due to severe eczema.
Common Impact on Both Conditions:
-
Treatment Management: It can take time and may be necessary to make lifestyle adjustments to adhere to treatment plans, medications, and skincare regimens.
-
Financial Burden: For some people, the costs of specialised skincare products, prescription drugs, medical visits, and treatments can be prohibitive.
-
Work or School Life: Symptoms may impact focus, output, attendance, or performance in the workplace or classroom.
-
Impact on Relationships: Because managing these conditions can have an emotional toll and alter social interactions, it may have an impact on relationships.
Managing psoriasis or eczema necessitates a multifaceted approach that addresses both physical and emotional symptoms. Seeking professional help, staying informed, and implementing coping strategies can significantly improve quality of life despite these chronic conditions.
Coping with Chronic Skin Conditions
Coping with chronic skin illnesses such as psoriasis and eczema necessitates a multifaceted approach to managing physical symptoms, emotional well-being, and overall quality of life. Education and understanding, skincare and treatment, stress management, lifestyle changes, support networks, mental well-being, acceptance and self-care, and seeking professional help are all useful coping techniques. Finding a balance between medical management, self-care, emotional support, and a positive outlook will help you manage and live well despite these problems.
Skincare Routines for Sensitive Skin
To avoid provoking responses or increasing sensitivity, sensitive skin skincare routines include moderate and non-irritating products. Here's a guideline for a sensitive skin skincare routine:
Morning Routine:
-
Cleanser: Use a gentle, fragrance-free, non-foaming cleanser designed specifically for sensitive skin. To avoid stripping natural oils, rinse with lukewarm water.
-
Toner (Optional): To rebalance the skin's pH levels, use an alcohol-free and soothing toner. Using a cotton pad, apply it gently.
-
Serum (Optional): If you must use a serum, choose one that is gentle and hydrating, with soothing ingredients such as hyaluronic acid or antioxidants. Apply a small amount to the skin and gently pat it in.
-
Moisturizer: Choose a moisturiser that is hypoallergenic, fragrance-free, and non-comedogenic for sensitive skin. For hydration, look for ingredients such as ceramides, glycerin, or shea butter.
-
Sunscreen: Finally, apply a broad-spectrum sunscreen with an SPF of 30 or higher. Select a mineral-based sunscreen containing zinc oxide or titanium dioxide, as they are less likely to irritate.
Evening Routine:
-
Makeup Removal: To remove makeup, use a soft makeup remover or micellar water. Avoid harsh rubbing and use products designed specifically for sensitive skin.
-
Cleansing: Cleanse the face with the same gentle cleanser used in the morning to remove impurities and pollutants. Hot water and abrasive scrubbing should be avoided.
-
Toner (Optional): If you are using a toner, repeat the steps from the morning.
-
Treatment (If Applicable): Follow your dermatologist's instructions for using any prescribed treatments, such as medicated creams or serums.
-
Moisturiser: To lock in moisture overnight, use the same gentle, hydrating moisturiser that you used in the morning.
Creating a skincare routine for sensitive skin entails using gentle, non-irritating products and being aware of how your skin reacts to various ingredients. Maintaining healthy, calm, and sensitive skin requires consistency and patience.
The Psychological Aspect of Skin Disorders
Skin problems, such as psoriasis, eczema, acne, vitiligo, and others, can have a significant psychological impact on people. Skin disorders' psychological components frequently extend beyond physical symptoms and can have a substantial impact on a person's mental well-being, self-esteem, body image, and general quality of life. Here are some essential psychological variables to consider:
Emotional Impact:
-
Stress and Anxiety: Living with chronic skin conditions can cause increased stress and anxiety, particularly during flare-ups or when confronted with social situations.
-
Depression: Persistent skin conditions may contribute to feelings of sadness, hopelessness, or depression due to the chronic nature of the condition and its impact on daily life.
-
Frustration and Helplessness: Feelings of frustration and helplessness can arise as a result of dealing with recurring symptoms or attempting various treatments without seeing significant improvement.
Body Image and Self-Esteem:
-
Self-consciousness: Visible skin changes can induce feelings of self-consciousness, embarrassment, or being judged by others, which can lead to a loss of confidence.
-
Negative Body Image: Skin disorders affecting visible areas can lead to negative body image perceptions, influencing how people perceive themselves.
Social and Relationship Impact:
-
Social Withdrawal: Social relationships may be impacted by social withdrawal or situation avoidance brought on by a fear of embarrassment or judgement.
-
Relationship Strain: Emotional distress or self-consciousness brought on by skin conditions may interfere with intimacy, dating, or relationships.
Coping Strategies:
-
Seeking Support: You can get emotional support and coping mechanisms by speaking with a therapist, attending support groups, or getting counselling.
-
Educating Others: Raising awareness of the illness among peers, family, and acquaintances can lessen stigma and foster greater compassion and understanding.
Comprehensive care requires an understanding of the psychological effects of skin disorders and taking appropriate action. Recognising these impacts and getting the right help are crucial since treating the emotional symptoms is just as important as treating the physical ones.
Beyond the Surface: The Broader Implications

Skin diseases can have greater repercussions that transcend beyond the physical and psychological elements of an individual's life, including society's perceptions, employment, and healthcare accessibility. Social stigma and perception, quality of life and everyday functioning, financial burden, access to healthcare, influence on mental health, advocacy, and awareness are some of the larger consequences of skin problems. Understanding the larger implications of skin disorders, beyond their physical manifestations and psychological impact, is critical for cultivating empathy, promoting inclusivity, and pushing for improved healthcare access and assistance for affected individuals. The creation of a more accepting and helpful society depends on initiatives to improve healthcare funding, alter public perceptions, and support people with skin conditions.
Autoimmune Elements in Psoriasis
Psoriasis is classified as an autoimmune condition because of an overactive immune system that kills healthy skin cells. The immune system plays a key role in the development of psoriasis, generating inflammation and fast skin cell turnover. Several autoimmune factors have a role in the pathophysiology of psoriasis:
-
Immune System Activation: In psoriasis, T cells, a type of white blood cell that plays an important role in the immune response, are abnormally activated. These T cells become overactive and cause skin inflammation. Abnormal T cell activation results in the release of pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-alpha), interleukins (IL-17, IL-23), and others. These cytokines promote inflammation by promoting rapid skin cell growth.
-
Inflammation and Skin Cell Turnover: Hyperproliferation occurs when the cytokines produced by activated T cells cause skin cells to reproduce at a faster rate, resulting in a rapid turnover of skin cells. Skin cells normally mature and shed over a few weeks, but in psoriasis, this process occurs in a matter of days. Psoriasis is characterised by an overproduction of skin cells (keratinocytes), which results in thick, scaly plaques.
-
Genetic Factors: Genetic factors influence the susceptibility to psoriasis. Individuals with a family history of psoriasis are more likely to develop the condition. Psoriasis is associated with certain human leukocyte antigen (HLA) genes, implying a genetic component in immune system dysfunction.
-
Triggers and Environmental Factors: Stress, infections, skin injury, certain medications, smoking, or hormonal changes can aggravate psoriasis by activating the immune response. Emerging research suggests a possible link between gut health and psoriasis, with imbalances in gut microbiota influencing the immune system and triggering or exacerbating psoriasis.
-
Autoimmune Component: While psoriasis is not an autoimmune disease, it shares characteristics with autoimmune diseases such as immune system dysregulation, inflammation, and an attack on the body's tissues (in this case, the skin).
Understanding the autoimmune nature of psoriasis has resulted in the development of targeted medicines, such as biologics, that selectively suppress immune system pathways implicated in the disease process. By modifying the immune response, these medicines try to minimise inflammation and regulate symptoms. The exact cause of psoriasis, on the other hand, remains complex and multifaceted, involving the interplay between genetic, environmental, and immune system components. Ongoing research into the underlying processes and potential new therapies for this persistent skin disorder is ongoing.
Environmental Influences on Eczema and Psoriasis
Environmental factors influence the development, aggravation, and management of eczema (atopic dermatitis) and psoriasis. Certain skin conditions, such as eczema (atopic dermatitis) and psoriasis, can be affected by environmental factors, which are common causes for both conditions as well as their treatment and prevention. While environmental impacts differ from person to person, recognising and addressing these factors can considerably aid in reducing the frequency and severity of eczema and psoriasis flare-ups. It is critical to work closely with healthcare providers to identify triggers and build personalised management programmes for various chronic skin disorders.















