Acne is a common skin condition where your skin follicles become blocked with oil and dead skin cells. It affects most people at some point in their lives. Acne is more prevalent in women than men, with more than 50% of women and 20% of men experiencing acne between the ages of 25- 45. The skin condition has a substantial impact on a patient's quality of life, affecting both self-esteem and psychosocial development. In this blog, we will learn some effective DIY tips for treating acne in 6 to 8 weeks and step out confidently with clearer skin.
What are the types of acne?

Acne is a common skin condition that occurs when hair follicles become clogged with oil, dead skin cells, and bacteria. It typically appears on areas of the skin with a higher concentration of oil glands, such as the face, neck, chest, shoulders, and back. To treat acne it helps to know which type of acne you’re dealing with as each type requires different treatment.
#1 Blackheads

These appear like small black or yellowish bumps that develop on the skin; they are not filled with dirt but are black because the inner lining of the hair follicle produces colour. Blackheads are most typically treated with over-the-counter medications, such as salicylic acid and benzoyl peroxide spot treatments. However, bumps that do not respond to treatment or are damaged as a result of at-home popping will necessitate a visit to a dermatologist. Our Chesterfield facility is particularly suited to help you treat blackheads, no matter how bad they appear.
#2 Whiteheads

Whiteheads, also known as closed comedones, are a form of acne lesion that appears on the skin's surface as small, flesh-colored or white pimples. They develop when hair follicles become clogged with a mixture of dead skin cells, oil (sebum), and, occasionally, microorganisms. Whiteheads, as opposed to blackheads, which have an open pore and look dark due to oxidation of trapped debris, have a closed pore that traps the contents beneath the skin. They appear like blackheads but are firmer and will not empty when squeezed.
#3 Papules

Papules are a type of acne lesion characterised by small, raised, solid bumps on the skin that do not have any visible fluid or pus. They usually appear as red or pink lumps and are classified as an inflammatory kind of acne lesion. Papules form when the hair follicles become irritated due to pore obstruction caused by excess oil, dead skin cells, and germs. They are small red bumps that may feel tender or sore.
#4 Pustules

Pustules are a type of acne lesion characterized by small, inflamed, raised bumps on the skin that contain visible pus. They are considered an inflammatory form of acne and are often tender to the touch. Pustules typically develop when pores become clogged with oil, dead skin cells, and bacteria, leading to inflammation and the formation of pus-filled lesions. They are bumps with a white tip in the centre and are caused by a build-up of pus.
#5 Nodules

Nodules are severe, deep-rooted acne lesions that form beneath the skin's surface. They are larger, more firm, and more painful than other types of acne lesions. Nodular acne is a severe form of acne that is frequently accompanied by substantial inflammation and possible scarring. They are large hard lumps that build up beneath the surface of the skin and can be painful and leave permanent marks
#6 Cysts
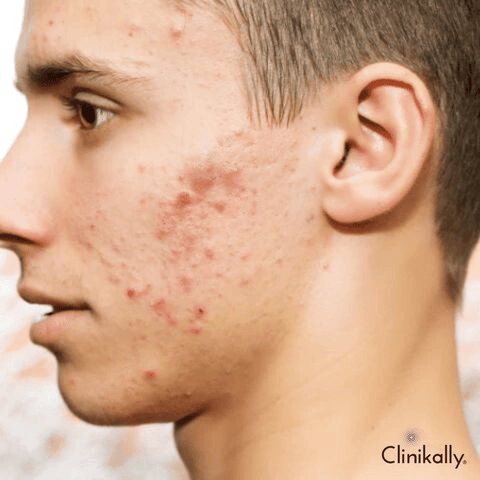
Cysts are severe and deep acne lesions that appear beneath the skin's surface as big, pus-filled lumps. They are one of the most severe types of acne and can be painful, inflammatory, and scarring. Because of its depth and potential for inflicting considerable skin damage, cystic acne frequently necessitates medical intervention. Its most severe type of spot is caused by acne, is largely filled with pus, and looks similar to boils. They can leave permanent marks when healed. This is the most painful grade of acne.
What causes acne?

Despite being the most common skin condition, acne still has many misconceptions surrounding it. For instance, the popular belief is that sexual activity can influence acne or that acne is caused by a poor diet. Some even suggest that eating chocolate can cause acne. However, there is no research supporting these claims. It is caused when sebum oil and dead skin cells plug the hair follicles causing an outbreak of lesions commonly called pimples or zits.
Here are some factors that can increase acne on the skin
-
Fluctuating hormone levels
-
Picking at acne sores
-
Getting too little sleep
-
Using some comedogenic cosmetics
-
Environmental stressors like air pollution
-
Medications like steroid medicines, lithium (used to treat depression and bipolar disorder) and drugs used to treat epilepsy
-
Wearing clothes or accessories that put pressure on the affected area of skin like headgear or a backpack
While stress is not directly related to acne, stress can increase existing acne.
Causes of acne in men

For men one of the main triggers of acne are fluctuations in the level of testosterone. Fluctuations in the level of testosterone in the body increases sebum production, along with clogged follicles that lead to bacterial growth resulting in acne breakout and inflammation. Facial hair on men can also serve as fertile ground for bacteria growth and trap oil. It is important to use a clean razor and moisturise before and after shaving. Acne in men can be caused by the same factors that cause acne in women. Here are some of the most common causes and contributing factors to male acne:
-
Hormonal Changes: During puberty, men's androgen hormones, such as testosterone, rise, stimulating the sebaceous glands to produce more oil. Excessive oil production can result in clogged pores and acne outbreaks.
-
Acne Predisposition: Men with a family history of acne may be more prone to developing the condition due to genetic factors.
-
Stress: Stress causes the body to release stress hormones like cortisol, which can affect the production of sebum and possibly aggravate acne in some men.
-
Environmental Factors: Acne can arise as a result of working in jobs where workers are exposed to oils, greases, or pollutants.
-
Lifestyle Factors: Consumption of high-glycemic-index foods, dairy products, or diets high in processed sugars and fats may aggravate acne breakouts in some people. Acne can be exacerbated by improper skin cleansing, the use of harsh skincare products, or the absence of a regular skincare routine.
-
Use of Specific Products: Certain men's skincare and haircare products may contain pore-clogging ingredients that can contribute to acne breakouts.
-
Irritation or Friction: Improper shaving techniques, the use of harsh shaving products, or repeated friction against the skin can cause irritation and aggravate acne in acne-prone areas.
-
Athletic Activities: Men who participate in sports or activities that cause excessive sweating may develop acne as a result of sweat and heat trapped in pores, resulting in clogged follicles.
Understanding the underlying causes of acne in males and using the right skincare practises can greatly aid in the prevention and management of acne breakouts.
Causes of acne in women

Acne is a growing problem among women, and they are more likely to be affected by adult acne than men are. This can be due to changes in hormonal levels that women have during certain times, including:
-
Women show flare-up of acne just before menstruation
-
In the first three months of pregnancy women show acne
-
Acne along with symptoms including weight gain and formation of small cysts inside the ovary due to polycystic ovary syndrome
Acne and toothpaste: Busting the acne myth

Popular rumour has it that applying regular toothpaste to your pimple might help to shrink it. The likely reason for this belief is because some ingredients found in toothpaste such as baking soda, alcohol, and hydrogen peroxide are said to be drying and might help in doing away with your zits. However this is a misconception, remember toothpaste is formulated for your teeth not the sensitive surface of your face. Toothpaste has a basic pH level and too much application can irritate your skin which has a natural pH level.
Acne treatment tips: What dermatologists recommend

While acne treatment is often complicated, there are several home remedies for pimples that will treat acne and even prevent acne breakouts from happening in the future.
#1 Go for acne-specific products

Use acne-specific products including face washes, moisturisers, and serums. Our skin care experts at Clinikally recommend products containing salicylic acid, benzoyl peroxide, and topical retinoids. You can shop such products from the convenience of home at Clinikally’s online inventory and get them delivered to your doorstep. Dermatologists recommend adding a Niacinamide serum for face along with a sunscreen with at least SPF 30. Apply the serum twice daily and protect your skin with sunscreen before stepping out. The serum prevents acne by reducing sebum production. It also reduces scarring and soothes inflammation.
#2 Avoid scrubs and excessive washing

Avoid facial scrubs at all costs. Also, repeated washing can lead to ‘Detergent Acne’. Here's why it's recommended:
Scrubs and Excessive Washing:
-
Irritation and Damage: Physical exfoliants, such as scrubs or harsh cleansing methods, can irritate the skin, disrupt its protective barrier, and cause micro-tears. This irritation may exacerbate acne and lead to increased inflammation.
-
Over-stripping Natural Oils: Excessive washing or the use of harsh cleansers can strip the skin's natural oils. This can cause the skin to produce even more oil in order to compensate, potentially exacerbating acne.
-
Skin Barrier Disruption: Scrubs or harsh cleansing can compromise the skin's barrier function, making it more vulnerable to bacteria, pollutants, and irritation.
-
Increasing Redness and Inflammation: Scrubbing skin that is prone to acne can exacerbate pre-existing lesions, possibly resulting in scarring.
Alternatives for Gentle Cleansing:
-
Non-Abrasive Cleaners: Use mild, non-comedogenic cleansers designed for skin that is prone to acne or is sensitive. For acne treatment, seek out ingredients such as salicylic acid or benzoyl peroxide.
-
Pat Dry Instead of Rubbing: To avoid unnecessary irritation, pat your skin dry gently with a clean towel after cleansing.
-
Limit Frequency: Wash your face twice a day, in the morning and evening. Excessive washing throughout the day can deplete the skin's natural oils.
-
Soft Washcloth or Clean Hands: When cleansing the face, use a soft washcloth or clean hands to avoid harsh scrubbing motions.
A dermatologist or skincare specialist can provide specialised advise on appropriate products and routines for your skin type and issues. They can recommend specialised cleansers, treatments, or lifestyle adjustments to properly manage acne without causing further skin irritation or damage.
#3 Do not touch or pick at problem areas

This can trigger affected areas and lead to infections and cause scarring. This also leads to PIH (post-inflammatory hyperpigmentation).
#4 Shower after exercise or work out

Activities like exercising or working out increase oil and sweat production, so shower regularly after exercise.
#5 Treat acne early

Early treatment can help prevent breakouts and target the root cause of acne.
#6 Manage stress effectively
Studies have shown that stress can flare acne. Manage and reduce stress in your day-to-day routines.
Treat acne and pimples with science

Acne is a common skin condition affecting most of us at some point in our lives. Keep in mind that what you think is a pimple may be another condition. You can get a dermatologist consultation online to get the best and personalised advice as per your skin type and concerns.
Clinikally is India’s first digital skin and hair clinic that lets you seamlessly consult dermatologists for personalised treatment plans that actually work. Effective treatment with products and formulations especially developed for use on acne and facial skin is a much safer bet and doesn’t need to cost you a fortune! Consistently using these treatments will keep your skin clear and healthy.
Understanding Acne Triggers and Prevention

Acne is a common skin condition caused by oil and dead skin cells clogging hair follicles. Understanding the causes and prevention techniques of acne can help you manage and reduce it. Here are some observations:
Triggers of Acne:
-
Hormonal Changes: Changes in hormone levels, particularly during puberty, menstrual cycles, pregnancy, or hormonal imbalances, can all contribute to acne.
-
Excessive Oil Production: Overactive sebaceous glands produce more oil (sebum), which can clog pores and cause acne.
-
Bacteria: Propionibacterium acnes, a skin bacteria, can multiply in clogged pores and cause inflammation and acne.
-
Genetics: A genetic predisposition can cause acne to run in families.
-
Diet: Research indicates that dairy, foods with a high glycemic index, and specific diets may make acne worse in some people, though these claims have not been proven conclusively.
-
Stress: Excessive stress can lead to hormonal changes that exacerbate acne.
-
Cosmetics and Skincare Products: A few types of makeup, skincare, and hair products have the potential to clog pores and cause breakouts of acne.
Prevention and Management:
-
Frequent Skincare Routine: Use a mild cleanser that is appropriate for your skin type (oily, dry, or combination) to gently cleanse your skin twice a day. Avoid harsh scrubbing that can irritate the skin.
-
Moisturise: Using a non-comedogenic moisturiser, even if you have oily skin, helps keep skin hydrated without clogging pores.
-
Avoid Touching Your Face: Touching your face can transfer dirt, bacteria, and oil from your hands, potentially exacerbating acne. Picking or squeezing pimples can result in scarring and further inflammation.
-
Manage Stress: Exercise, meditation, yoga, and deep breathing can all help reduce stress, which in turn can help reduce acne flare-ups.
-
Healthy Diet: While individual responses to diet vary, eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins may help some people manage acne better.
-
Non-Comedogenic Products: To avoid pore blockages, choose makeup, sunscreen, and skincare products that are labelled as non-comedogenic or oil-free.
-
Seek Professional Help: If acne persists or is severe, consider consulting a dermatologist. They can provide personalized treatment plans such as topical treatments, oral medications, or procedures like chemical peels or laser therapy.
Never forget that maintaining and preventing acne requires consistency in skincare practises and lifestyle adjustments. It is important to find a routine that suits your skin type and takes care of your particular concerns because what works for one person might not work for another.
Dietary factors and acne

The association between nutrition and acne has received a lot of attention, although the specific impact of diet on acne is not totally known. Several dietary elements, however, have been proposed to potentially influence the development or severity of acne:
-
High-Glycemic Index (GI) Foods: High glycemic index foods, such as white bread, sugary snacks, processed foods, and some cereals, can trigger blood sugar rises. These increases may stimulate hormones, potentially exacerbating acne by increasing oil production and inflammation.
-
Dairy Products: Some research imply a link between dairy consumption, particularly skim milk, and acne. It is thought that hormones included in dairy products contribute to acne formation. More research, however, is required to validate this association and understand the underlying mechanisms.
-
Omega-6 Fatty Acids: Inadequate omega-6 to omega-3 fatty acid ratios in the diet may increase inflammation, potentially exacerbating acne. Certain vegetable oils (such as soybean and maize oil) and processed foods are high in omega-6 fatty acids.
-
Food Sensitivities: Certain foods may cause immunological reactions or sensitivities in some people, resulting in skin irritation and acne. Gluten, some nuts, seafood, and particular chemicals or preservatives are common culprits.
-
Antioxidants and Anti-Inflammatory Foods: Antioxidant-rich diets (e.g., fruits and vegetables) and anti-inflammatory foods (e.g., fatty fish, almonds, olive oil) may help reduce inflammation and possibly improve general skin health, including acne.
-
Water Intake: Staying hydrated is critical for overall skin health. Drinking plenty of water aids in the removal of toxins and keeps the skin moisturised, potentially lowering the severity of acne.
It is important to note that the effect of nutrition on acne varies greatly between individuals. What causes acne in one individual may not cause acne in another. Aside from these variables, skincare practises, hormone cycles, and heredity all affect the development of acne.
Tips for Managing Diet-Related Acne:
-
Keep a Food Diary: Track your eating habits to see if there are any correlations between particular foods and breakouts of acne.
-
Healthy Diet: Make sure your diet is well-balanced by consuming lots of fruits, vegetables, lean meats, and whole grains, and minimising processed foods, sugary snacks, and high-glycemic foods.
-
Individual Experimentation: If you think that a certain food makes your acne worse, think about gradually cutting it out and seeing if your skin changes.
-
Speak with a Professional: If you think that a particular food is causing your acne, you should talk to a registered dietitian or another medical professional for individualised guidance.
Although diet may have an effect on acne, it is important to remember that effective acne management also requires a healthy lifestyle, appropriate skincare, and consultation with healthcare providers.
Role of hormones in acne
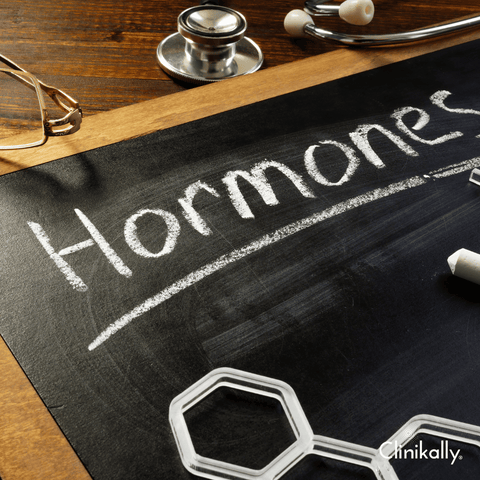
Hormones play a significant role in the development of acne. Fluctuations in hormone levels, particularly androgens (male hormones found in both males and females), can influence the activity of the sebaceous glands in the skin. This increased activity can lead to an overproduction of oil (sebum), which can clog pores and create an environment conducive to acne formation when combined with dead skin cells. Several key hormonal factors contribute to acne:
-
Androgens: Androgens, which include testosterone, are naturally occurring hormones found in both males and females. Increased androgen levels, especially during adolescence, can cause the sebaceous glands to generate more oil. Excessive oil production can cause clogged pores and an increase in the incidence of acne outbreaks.
-
Hormonal Fluctuations: Acne can be influenced by hormonal variations during menstrual cycles, pregnancy, and menopause. Because of hormonal shifts, women may develop acne flare-ups before their menstrual cycles. Hormonal abnormalities, such as polycystic ovarian syndrome (PCOS), can result in elevated androgen levels and acne.
-
Stress Hormones: Stress can cause the release of stress hormones such as cortisol, which can accelerate the production of oil in the skin. Stress-induced increases in oil production can contribute to acne development or aggravation.
-
Hormonal Treatments: Some medications or therapies that impact hormone levels, such as oral contraceptives (birth control pills) containing oestrogen and progestin, may help some people manage their hormones and improve their acne. Anti-androgen medicines, which reduce androgen activity, may also be recommended to manage hormone-related acne.
-
Hormonal Influence on Specific Types of Acne: Deep, cystic pimples along the jawline, chin, and lower face are common symptoms of hormonal acne. This type of acne is generally resistant to topical therapies and may necessitate hormone therapy under the supervision of a doctor.
Understanding the hormonal influence on acne is critical, especially for people who have persistent or severe acne that appears to be hormonal in nature. Dermatologists or other healthcare specialists can assess hormonal issues and propose suitable treatments, such as oral contraceptives, anti-androgen medicines, or other hormone-balancing therapy. Combining hormone management with proper skincare and lifestyle changes can be successful in controlling and minimising the severity of hormonal acne.
Acne from cosmetics: Comedogenic ingredients to avoid

Cosmetic acne, also known as acne cosmetica, arises when particular components in makeup, skincare, or haircare products clog pores, causing acne to develop or exacerbating existing acne. To reduce the risk of acne from cosmetics, be cautious of comedogenic ingredients—substances that are more likely to clog pores and cause breakouts. The following are some comedogenic ingredients to avoid:
Comedogenic Ingredients to Watch Out For:
-
Isopropyl Myristate: Found in moisturisers and foundations, this ingredient can be highly comedogenic for some people.
-
Algae Extract: Found in a variety of skincare and makeup products, it has been linked to breakouts in sensitive people.
-
Cocoa Butter: A common ingredient in moisturisers and lip balms, cocoa butter has a higher comedogenic rating and may clog pores in some people.
-
Coconut Oil: Although some people find great results with it, others may develop acne due to its higher comedogenic rating.
-
Wheat germ oil: Often found in skincare products, this ingredient has a strong tendency to clog pores.
-
Lauric Acid: Found in some oils, such as coconut and palm kernel oils, it may cause breakouts in some people.
-
Almond oil: Although it helps certain skin types, it can cause acne in others due to its comedogenic properties.
-
Soybean oil: Having a moderate to high comedogenic rating, it is a common ingredient in skincare and cosmetic products.
-
D&C Red dyes: Sensitive people may experience worsening acne when exposed to certain red dyes found in cosmetics, such as D&C Red 30 and D&C Red 36.
Tips to Avoid Acne from Cosmetics:
-
Examine Labels: Seek for products bearing the labels "oil-free" or "non-comedogenic." These are designed to be less prone to break you out in acne.
-
Patch Test: Use a small patch test area of your skin to check for any negative reactions before using a new product.
-
Avoid Using Thick Makeup: Thick, heavy foundations or concealers can clog pores more easily. Choose lighter, water-based products instead.
-
Choose Water-Based Formulations: When compared to oil-based alternatives, water-based or gel-based products are less likely to clog pores.
-
Fragrance-Free Products: Fragrances can irritate the skin and aggravate acne. Consider using fragrance-free or hypoallergenic products.
-
Regularly Clean Brushes and Applicators: Dirty makeup brushes and applicators can harbor bacteria, leading to acne. Clean them regularly.
-
Remove Makeup Properly: Before going to bed, make sure you thoroughly remove your makeup with a gentle cleanser that is appropriate for your skin type.
-
Consult a Dermatologist: If you have persistent acne caused by cosmetics, see a dermatologist for personalised recommendations.
Being aware of the ingredients in your cosmetics and selecting products labelled non-comedogenic or suitable for acne-prone skin can significantly reduce the risk of acne caused by makeup or skincare products.
Post-Acne Care and Scar Treatment

Post-acne care plays an important role in scar management and skin repair following acne breakouts. Following are some methods and treatments for post-acne care and scar treatment:
Skincare Routine:
-
Gentle Cleansing: To keep the skin clean without causing irritation, use a mild, non-comedogenic cleanser twice daily.
-
Moisturization: Use a non-comedogenic moisturiser to keep the skin hydrated and help it heal.
-
Sun Protection: To prevent further darkening or discoloration of acne scars, use a broad-spectrum sunscreen with an SPF of 30 or higher.
-
Avoid Picking or Squeezing: Avoid picking or squeezing at acne lesions, as this can worsen inflammation and increase the risk of scarring.
Scar Treatment Options:
-
Topical Treatments: By encouraging cell turnover and collagen production, prescription retinoid creams, such as tretinoin, can help reduce the appearance of acne scars. Product formulations with BHAs like salicylic acid or AHAs like glycolic acid may help to improve the texture of acne scars and provide a light exfoliation. The appearance of post-inflammatory hyperpigmentation can be lessened with the help of topical vitamin C serums.
-
Chemical Peels: Chemical peels entail applying a chemical solution to the skin, which exfoliates the outer layers and gradually reduces the visibility of acne scars.
-
Microneedling: Also known as collagen induction therapy, microneedling produces controlled micro-injuries in the skin to increase the production of collagen and minimise the appearance of scars.
-
Laser Therapy: Several laser types, including intense pulsed light (IPL) and fractional lasers, can target particular skin layers to reduce the visibility of acne scars.
-
Dermal Fillers: Hyaluronic acid is one injectable dermal filler that can temporarily fill in depressed acne scars to give the skin a smoother appearance.
-
Steroid Injections: Corticosteroid injections can help relieve inflammation and flatten the scar tissue in raised or hypertrophic scars.
-
Surgical Treatments: Dermatologists and plastic surgeons may recommend punch excision, subcision, or skin grafting in severe cases to treat deep or extensive acne scars.
Patience and Consistency:
-
The kind and intensity of scars can affect the outcome of acne scar treatment, which frequently requires patience. Maintaining a skincare regimen and treating patients according to dermatologists' recommended treatment plans requires consistency.
-
Combine various scar treatment methods according to the kind of scars you have, and speak with a dermatologist or skincare specialist to figure out the best course of action for your particular skin type.
Always seek professional advice before beginning any new treatment, especially for more invasive procedures. Based on your needs, a dermatologist can evaluate your skin and recommend the best course of action for treating acne scars.
Best treatments for acne scars

Treatment for acne scars can involve a variety of methods, depending on the type, severity, and depth of the scars. The following are some of the most effective treatments for various types of acne scars:
-
Atrophic Scars (Depressed Scars): Injectable hyaluronic acid fillers can temporarily fill in depressed scars, resulting in a smoother skin surface. Microneedling injures the skin in a controlled manner, stimulating collagen production and improving the appearance of atrophic scars. Subcision is a surgical technique that separates deeper tissues from scars by passing a needle or blade beneath the scar. As a result, the depressed scar is elevated. Fractional laser therapy is a skin-specific treatment that stimulates collagen production in specific areas of the skin to improve the appearance of atrophic scars.
-
Hypertrophic or Keloid Scars (Raised Scars): Corticosteroid injections can help reduce elevated scars by reducing inflammation and limiting the creation of new collagen. Over time, silicone gel and sheets can help flatten and soften hypertrophic scars. Laser treatments such as pulsed dye lasers or fractional lasers can help to reduce raised scars.
-
Post-Inflammatory Hyperpigmentation (PIH): Prescription retinoids can help fade discoloration and improve skin texture. Topical vitamin C serums can aid in the reduction of hyperpigmentation and the stimulation of collagen production. Chemical peels can help with exfoliation and hyperpigmentation reduction.
-
Ice Pick Scars (Deep, Narrow Scars): Punch excision is the surgical removal of individual ice pick scars followed by suture closure of the incision. A method of inducing controlled inflammation and stimulating collagen formation by injecting high concentrations of TCA directly to ice pick scars.
Important Considerations:
-
Professional Consultation: It is critical to seek the advice of a dermatologist or skincare professional who can assess your scars and recommend the best treatment plan for your specific needs.
-
Combination Therapies: For treating various types of acne scars, a combination of treatments often produces the best results.
-
Patience and Consistency: Treating acne scars takes time, and results may vary. Consistent adherence to treatment plans and proper skincare is essential for achieving desired outcomes.
Before undergoing any acne scar treatment, always consult with a healthcare professional about the potential risks, benefits, and expected outcomes.
Importance of moisturizing acne-prone skin

Moisturising acne-prone skin is crucial, despite common misconceptions that it may exacerbate acne. Here's why moisturising is important for acne-prone skin:
-
Maintains Skin Barrier: Acne-prone skin is frequently dehydrated as a result of the usage of acne treatments such as benzoyl peroxide or salicylic acid. Moisturising restores the moisture balance of the skin without blocking pores. A moisturised skin barrier is better able to guard against environmental irritants and germs that might worsen acne.
-
Prevents Excessive Oil Production: When the skin becomes overly dry as a result of aggressive acne treatments, the body may adjust by creating more oil, thereby exacerbating acne. Proper moisturization aids in the prevention of this rebound effect.
-
Reduces Irritation and Inflammation: Some acne treatments can make your skin dry, red, or flaky. A good moisturiser can soothe and relax inflamed skin while also lowering inflammation.
-
Choosing the Right Moisturizer: Choose acne-prone skin moisturisers that are non-comedogenic, oil-free, or gel-based. These products are less prone to clogging pores. Look for moisturisers that contain hyaluronic acid or glycerin, which hydrate the skin without adding excessive oil.
Tips for Moisturising Acne-Prone Skin:
-
Consistency: To keep skin hydrated on a regular basis, moisturise twice a day after cleansing.
-
Light Application: Apply a pea-sized amount, especially to oily areas, to prevent feeling greasy or overly moisturising.
-
Patch test: To make sure new moisturisers do not irritate or cause breakouts, test them on a small portion of your skin.
-
Avoid Irritants: Avoid products that are heavy, fragranced, or excessively oily, as these may aggravate acne.
Remember that everyone's skin is different, so finding the right moisturiser may require some trial and error. A dermatologist or skincare professional can assist you in selecting the best moisturiser for your specific acne-prone skin type.
Sunscreen: A must for acne-prone and scarred skin

Yes, sunscreen is an essential part of skincare, especially for acne-prone and damaged skin. Here's why sunscreen is vital for acne management and scar prevention:
-
Protection Against Post-Inflammatory Hyperpigmentation (PIH): Sun exposure can aggravate the appearance of acne scars by causing post-inflammatory hyperpigmentation (PIH), which causes scars to darken and become more visible.
-
Minimizes UV-Induced Inflammation: Sun exposure can cause skin inflammation, which can aggravate acne and slow the healing of existing scars.
-
Balances Hyperpigmentation: By halting the further darkening of pre-existing hyperpigmentation or scars, regular sunscreen use can help maintain an even skin tone.
Sunscreen Tips for Acne-Prone and Scarred Skin:
-
Non-Comedogenic Formulas: To prevent clogging pores and triggering breakouts, opt for oil-free or non-comedogenic sunscreens that are specifically formulated for skin prone to acne.
-
SPF 30 or Higher: To protect yourself from UVA and UVB rays, use a broad-spectrum sunscreen with an SPF of 30 or higher.
-
Application Technique: Use a light hand when applying sunscreen to prevent irritating or exacerbating sensitive skin or acne-prone areas.
-
Reapplication: Reapply sunscreen every two hours, particularly if you spend a lot of time outside or in the sun.
-
Take into Account Particular Ingredients: Seek for sunscreens with components like titanium dioxide or zinc oxide, as these are less likely to irritate skin that is prone to acne or is sensitive.
Importance of Daily Use: The application of sunscreen every day, regardless of weather or indoor/outdoor activities, is critical for the health of acne-prone and scarred skin.









































